The COVID-19 pandemic, which was declared a Public Health Emergency (PHE) under Section 319 of the Public Health Service (PHS) Act, brought in emergency declarations by the US government, legislative measures through Congress, and regulatory actions through agencies such as the Centers for Medicare & Medicaid Services (CMS). Numerous modifications were introduced to respond to the pandemic and healthcare providers were allowed maximum flexibility to streamline care delivery and ensure uninterrupted access to care during this time. As the situation has been improving, and considering the current COVID-19 trends, the Department of Health and Human Services (HHS), in January this year, decided to transition away from the PHE phase. And May 11, 2023, is going to mark the end of the federal PHE for COVID-19.
In light of this recent announcement and with the transition date just around the corner, the healthcare system has been preparing itself to adapt to the new guidelines for the post-COVID PHE phase.
This article is to throw light on the various adjustments in regulations that had been made during the PHE, how many of these changes are due to expire soon with the May 11 cutoff, and what will continue to be extended. It also covers the impact of these modifications on the key stakeholders of the healthcare system—the providers and payers, providing insights into how they can adapt to the new laws successfully in the post-PHE landscape.
Amidst all the reforms and policy changes, addressing COVID-19 continues to remain a significant public health priority for the administration.
End of COVID-19 PHE – What Stays and What Changes
Let us now see what is changing and what is not with the end of PHE on May 11, 2023, and which of the waivers will continue to be extended post-PHE.
COVID-19 Vaccines, Testing, and Treatment
What’s Changing
- Medicaid coverage for COVID-19 vaccinations, testing, and treatment of uninsured individuals from the 18 states and US territories that opted for providing free coverage during the pandemic, will end when the PHE ends.
- After the expected end of the PHE on May 11, 2023, mandatory coverage for over-the-counter and laboratory-based COVID-19 PCR and antigen tests will end. However, coverage will vary depending on the health plan.
- If private insurance chooses to cover both of these that are mentioned above, cost sharing, prior authorization, or other forms of medical management may be required.
What’s Not Changing
- People with Medicare coverage will continue to have access to COVID-19 vaccinations without cost-sharing even after the end of the PHE.
- Those with traditional Medicare will continue to receive COVID-19 PCR and antigen tests with no cost sharing when the test is ordered by a physician or certain other healthcare providers, such as physician assistants and certain registered nurses, and performed by a laboratory.
- There is no change in Medicare coverage of treatments for those exposed to COVID-19 once the PHE ends, and in cases where cost sharing and deductibles apply now, they will continue to apply.
- The end of the COVID-19 PHE does not change access to oral antivirals, such as Paxlovid and Lagevrio.
- In the case of Medicaid and Children’s Health Insurance Program (CHIP), states must provide coverage without cost sharing for COVID-19 vaccinations, testing, and treatments through the last day of the first calendar quarter that begins one year after the last day of the COVID-19 PHE. As COVID-19 PHE is expected to end on May 11, 2023, this coverage requirement will end on September 30, 2024.
- In the case of private health insurance too, the transition forward from the PHE will not change how treatments are covered, and in cases where cost sharing and deductibles apply now, they will continue to apply.
- Most forms of private health insurance must continue to cover COVID-19 vaccines furnished by an in-network healthcare provider without cost sharing. However, people with private health insurance may need to pay part of the cost, if an out-of-network provider vaccinates them.
Access to Telehealth Services
- During the PHE, individuals with Medicare had broad access to telehealth services, including in their homes, without geographic or location limits. Under the Consolidated Appropriations Act 2023, many of these telehealth flexibilities have been extended through December 31, 2024, including –
- People with Medicare can access telehealth services from any geographic location in the United States, and not just in rural areas.
- People with Medicare can stay in their homes for telehealth visits that Medicare pays for rather than traveling to a healthcare facility.
- Certain telehealth visits can be delivered audio-only (such as a telephone) if someone is unable to use both audio and video, such as a smartphone or computer.
- Medicare Advantage plans may offer additional telehealth benefits.
- Additionally, after December 31, 2024, when these flexibilities expire, some Accountable Care Organizations (ACOs) may offer telehealth services that allow primary care doctors to care for patients without an in-person visit, no matter where they live.
- For Medicaid and CHIP, telehealth flexibilities are not tied to the end of the PHE and have been offered by many state Medicaid programs long before the pandemic. Coverage will ultimately vary by state.
- For private insurers, coverage for telehealth and other remote care services will vary on private insurance plans after the end of the PHE as it is currently.
Other CMS Waivers and Administrative Flexibilities
- The standard CMS Blanket Waivers that have been made available to several categories of providers will be discontinued at the end of the PHE. Some of these include:
- Waiver of the requirement for three-day prior in-patient hospitalization to qualify for Medicare coverage of their post-hospitalization care at a skilled nursing facility.
- Waiver of the requirement that Critical Access Hospitals (CAHs) limit the number of inpatient beds to 25 and hospital stays to no longer than 96 hours on average.
- Waiver to allow acute care patients to be housed in other facilities, such as ambulatory surgery centers, inpatient rehabilitation hospitals, hotels, and dormitories.
- The Acute Hospital Care at Home initiative that allows flexibility for hospitals to expand their capacity to provide inpatient care in an individual’s home has been extended through December 31, 2024, under the Consolidated Appropriations Act, 2023. If an individual is receiving care in a participating hospital and meets the requirements to receive inpatient care at home, they can continue to get it.
- The CMS had granted individual, time-limited waivers to help nursing home facilities to overcome pandemic-related workforce shortages and enable staff undergoing Nurse Aide Training to deliver care. All nursing aide training emergency waivers for states and facilities will end at the end of the PHE, which is expected on May 11, 2023.
- The flexibility extended on direct supervision through virtual presence, facilitating the provision of telehealth services, will expire on December 31, 2023.
- The emergency waiver that allowed Certified Registered Nurse Anesthetists (CRNAs) to practice to the full extent of their licensure without physician supervision, at the discretion of the hospital or Ambulatory Surgical Center (ASC) and state law, during PHE, will be lifted at the end of the PHE.
- Apart from these, a significant number of other emergency waivers related to health and safety requirements will expire at the end of the PHE, such as, the time frame to complete a medical record at discharge was extended because of the large volume of patients and also clinicians being away from direct patient care for extended period of time, would now go back to the standard timeframe.
- The condition for individuals to be continuously enrolled in Medicaid culminated on March 31, 2023, and hence is no longer linked to the end of PHE. The temporary Federal Medical Assistance Percentage (FMAP) increase has also been phased down since the beginning of April 1, 2023, and is expected to end on December 31, 2023.
How the End of COVID PHE is Expected to Impact the Healthcare System
The announcement of the expiry of the COVID PHE and the new guidelines and policy changes by CMS is expected to have a significant impact across the healthcare continuum. For instance,
- A slowdown in precautionary measures, such as wearing a mask, social distancing, and hand hygiene, among the public
- A slack in testing and overall surveillance efforts, leading to reduced detection of cases and delayed contact-tracing
- A relaxed approach towards addressing supply chain issues and future staffing shortages, ensuring sufficient resources for healthcare workers, and general preparedness to deal with any kind of future surge in demand by hospitals.
The providers and payers may also face some challenges around healthcare utilization, funding, and staffing as they adapt to the adjustments. Some of these potential challenges include –
• Increase in Demand for Healthcare Services
With the end of the PHE, those who avoided medical visits and tests due to the fear of contracting the COVID virus are likely to return to their routine checkups and treatment plans. This shift in healthcare utilization may lead to longer waiting times for patients and an increase in pressure on the healthcare system.
• Financial Limitations
The decrease in COVID-related funding, reimbursement modifications, and withdrawal of financial support from the government post the end of PHE may pose some level of financial challenges for healthcare providers.
• Staff Shortages
The workload on the healthcare workers and physician burnout during COVID-19 was phenomenal. And the end of PHE is likely to result in staff shortages for healthcare providers as many may leave the medical field and transition to other job areas. Therefore, the work pressure on those who remain is expected to increase.
Preparing to Adapt to the Post-PHE Changes
As the healthcare system transitions, both providers and payers must prepare themselves to respond strategically to the upcoming reformations in the post-COVID PHE landscape. A proactive approach by providers and payers that includes modifying coverage policies, re-evaluating reimbursement models, addressing social determinants of health, and promoting preventive care, can ensure patients continue to receive high-quality care while organizations sustain the changeover successfully.
Steps to Take: How Providers and Payers Can Respond to the Evolving Healthcare Landscape
- To respond to new COVID cases in the post-PHE phase and be prepared to contain future outbreaks more efficiently, healthcare providers and payers must continue with their surveillance efforts. even after the expiry of the PHE.
- Providers must consider investing in local or regional supply chain networks, adopt new inventory management strategies, and collaborate with other stakeholders to ensure that critical medical supplies are available whenever and wherever needed.
- Besides, healthcare providers and payers must partner with public health agencies, community-based organizations, and patient advocacy groups, to promote health awareness campaigns. This would encourage healthy behavior among communities and curb the spread of diseases like COVID-19 in the future to ease the burden on the healthcare system.
- Payers must evaluate their reimbursement models and carry out necessary modifications in coverage, introducing benefit policies to ensure that they are sustainable in the post-COVID healthcare landscape. This may include changes to reimbursement rates, as well as new care delivery approaches like value-based care that incentivize high-quality, cost-effective care and bring new payment models.
- The pandemic has highlighted the importance of addressing social determinants of health (SDoH), such as food insecurity, housing instability, demographics, etc., and also behavioral and mental health. Both providers and payers can play a significant role in addressing these issues by investing in programs that revolve around social determinants of health and partnering with community organizations to support exposed populations.
- Providers and payers must also actively promote preventive care and invest in programs that encourage healthy behavior and precautionary measures, such as vaccinations and cancer screenings. This can help in reducing the long-term impact of COVID on population health and bring down overall healthcare costs.
- Most importantly, both providers and payers must embrace technology that can become the key driver for all the above initiatives. By adopting new and relevant strategies for digital transformation and embracing modern technologies like telemedicine, remote patient monitoring, data analytics & AI (Artificial Intelligence), they can enhance workflow efficiencies, avoid physician burnout, and ease the administrative burden—all that collectively translates into better care delivery, reduced costs, and enhanced patient outcomes.
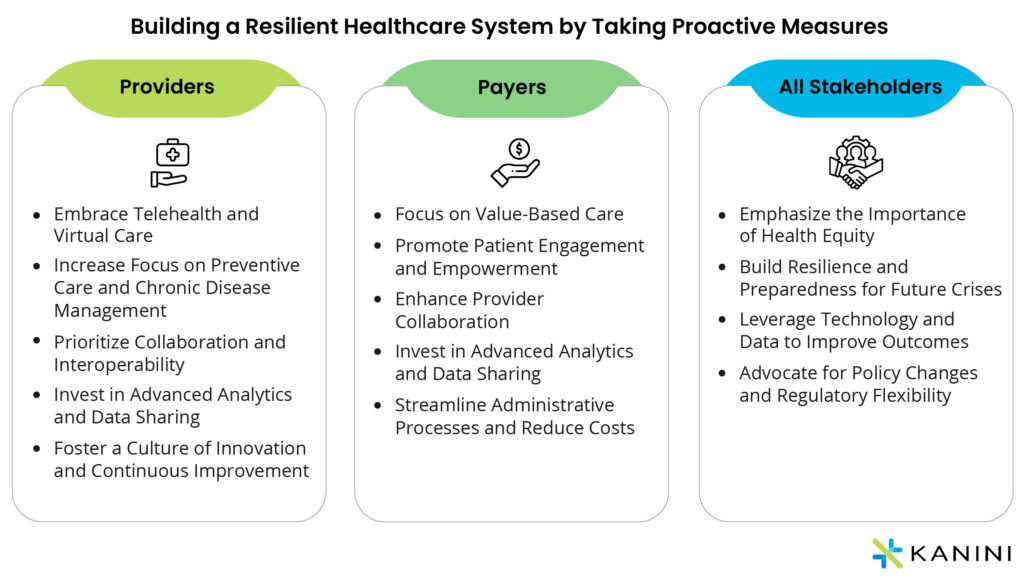
| Providers | Payers | All Stakeholders |
|---|---|---|
| Embrace Telehealth and Virtual Care | Focus on Value-Based Care | Emphasize the Importance of Health Equity |
| Increase Focus on Preventive Care and Chronic Disease | Promote Patient Engagement and Empowerment | Build Resilience and Preparedness for Future Crises |
| Prioritize Collaboration and Interoperability. | Enhance Provider Collaboration | Leverage Technology and Data to Improve Outcomes |
| Invest in Advanced Analytics and Data Sharing | Invest in Advanced Analytics and Data Sharing | Advocate for Policy Changes and Regulatory Flexibility |
| Foster a Culture of Innovation and Continuous Improvement | Streamline Administrative Processes and Reduce Costs | - |
The Post-PHE Journey Ahead with Technology as a Key Enabler
Technology has become a key enabler in sustaining the shift successfully after its proven prowess in tracking and managing vaccinations for populations across countries during peak COVID times. The role of technology is extraordinary in monitoring patient health remotely, contact tracing, automating processes, digitizing health records, improving diagnoses, drawing data-driven analyses, and making predictions for the future of healthcare.
Our next blog post – The Role of Technology in Addressing Healthcare Emergencies and Policy Changes – will uncover how a strategic investment in new-age technology solutions becomes a must to improve patient care and make data-driven decisions to handle any irregularities or variations during healthcare emergencies, and how technology helps in building a resilient healthcare system that can easily adapt to policy changes like the end of COVID 19 PHE in the US.
Progressing with a forward-thinking approach, under the right guidance from technology partners and consulting experts, healthcare providers and payers can quickly acclimatize and withstand the impact of the healthcare crisis. Reach out to us to know more about how our advanced technology solutions and consulting services at KANINI are enabling healthcare enterprises to adapt to the changes in healthcare.
Author

Neha Sinha
Neha is leading the business consulting efforts for the Healthcare BU at KANINI. She brings on board 15+ years of experience in driving various critical functions such as Business Analysis, Presales, Client Relationships, and Domain Consulting. Neha has spent over a decade working with healthcare clients and engagements in the US market.








