“In every other industry, you get to see prices up front. Healthcare should be no different. It’s time for transparency.”
Marty Makary, M.D., Surgeon, a Public Policy Researcher at Johns Hopkins University, and Author of “The Price We Pay” and “Unaccountable” (He writes for The Washington Post and The Wall Street Journal)
The CMS Mandate for Transparent Cost Estimation and Disclosures
“Transparency can play a significant role in reducing healthcare disparities by giving patients more information to make decisions that align with their individual needs.”
– American Medical Association
- In-network provider-negotiated rates based on the contract for all covered items and services.
- Historical data that shows both billed and allowed amounts for all covered items and services set by out-of-network providers, including prescription drugs.
- Negotiated rates and historical net prices for prescription drugs set by in-network providers. Currently, HHS has delayed enforcing this piece of requirement indefinitely, and it is pending additional rulemaking.
“The MRFs are wonderful because, for the first time, the industry has a normalized source of common and comprehensive data that software tools such as decision support apps can consume to powerfully help consumers make choices.”
– Jay Sultan (Healthcare Innovation Executive, Operating Partner-United Generations Capital)
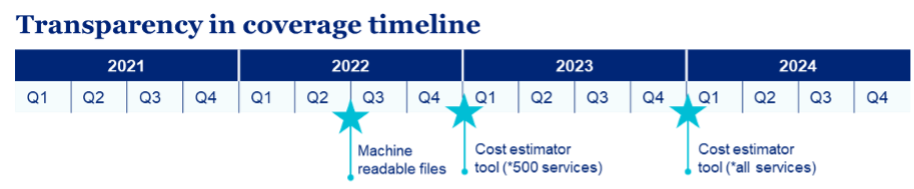
Since January 1, 2023, health plans have been required to provide a cost estimator online tool to their plan participants, beneficiaries, enrollees, or their authorized representatives. The objective is to disclose the cost-share estimates for 500 shoppable services covering areas such as imaging services (e.g., CPT Code – 78306), laboratory tests (e.g., CPT Code – 87205), elective surgical procedures (e.g., MS-DRG Code – 470), and preventive screenings such as mammograms and colonoscopies (e.g., HCPCS Code – G0120)
For plan years beginning on or after Jan. 1, 2024, the online tool must provide cost-share estimates for all covered services to help consumers understand healthcare costs and their estimated cost-sharing liability based on their benefits and deductible and/or out-of-pocket accumulations, as well as compare costs across providers before obtaining care. This self-service online tool should be able to provide below listed information/features as applicable:
- Both in and out-of-network estimated costs (out-of-network costs may be dollars or percent).
- Allow members or personal representatives to search based on the billing code or description of the billing code.
- Advise members of their status towards the deductible, out-of-pocket maximums, and their accumulations to date.
- Provide a cost estimate in paper format at the member’s request.
The Challenge of Large Volumes of MRF Data: One of the Biggest Roadblocks in the TIC Endeavor
A Step-wise Approach to Addressing the Big Data Challenge in MRF Analysis
Data Integration and Centralization
- A centralized repository that integrates data from diverse sources.
- Data standardization to ensure consistent coding systems, terminologies, and formats across different data sources.
Real-time Data Updates
- Automated mechanisms to update information in real-time to capture the changes that occur due to negotiations, guidelines, or other factors.
- Data validation processes to ensure data accuracy and prevent discrepancies.
Data Privacy and Security
- Robust data encryption, access controls, and audit trails to protect sensitive patient and financial information.
Data Quality Management
- Data quality tools and processes to identify and rectify errors, inconsistencies, and inaccuracies in pricing data.
- Data profiling and cleansing techniques to improve the reliability of the presented pricing information.
Data Visualization and Interpretation
- User-friendly data visualizations, such as charts, graphs, and interactive dashboards.
- Clear explanations and annotations to enhance the interpretation of complex structures.
AI-driven Recommendations and Forecasting
- Recommendations on plans, pricing, and providers using the extensive open data ingested into the data lake.
- An AI-based Q&A platform allowing users to ask questions about plans, providers, services, negotiation rates, etc.
- Forecasting models, predicting the availability of a specific drug for a specific season.
Upholding the Promise of Healthcare Pricing Transparency for a Better Future
Author









